This is a fascinating article brought to my attention by Barb Farlow, who we interviewed in For the love of Annie.
The role of a pediatric ethics committee in the newborn intensive care unit is published in the Journal of Perinatology this month and looks at ethical issues related to parent authority and best interest of the child. A couple of cases are presented, including one of an infant with Trisomy 13 who needs heart surgery. Historically, this type of surgery wouldn't be performed because Trisomy 13 is associated with early infant mortality. The author notes, however, that early death may be in part because efforts are not made to save these children.
Help BLOOM grow!
Popular Posts
-
By Tina Szymczak In 2010, our darkest times as a family, I began to use the analogy of a swimming pool to describe the difficult parts ...
-
By Louise Kinross Today is Bell Let’s Talk day and we want to join the dialogue by talking about mental health and parenting childre...
-
By Sue Robins In the foyer of every elementary school there's a gaggle of moms standing in a tight circle, waiting ...
-
By Louise Kinross Disability is personal. It’s part of identity. When your child has significant disabilities, it becom...
-
About half of the parents and professionals who've filled out our BLOOM survey so far have asked for more stories on families raisin...
-
Many of you will remember our interview with filmmaker Kelly O'Brien, whose film Softening documents life with her s...
-
By Louise Kinross “When I was seven, I asked when I was going to get my chair,” says Elijah Wangeman, 14 (above left), in an unedit...
-
By Louise Kinross I read R. J. Palacio’s book Wonder —about a boy called Auggie with a craniofacial condition that elicits stares an...
-
By Louise Kinross A few year's back it was suggested to me that a great co-op placement for my son was to work in a school separ...
-
By Louise Kinross David James Savarese, known as DJ or Deej, has autism and doesn't speak. As a young child, he was placed in foster ...
Total Pageviews
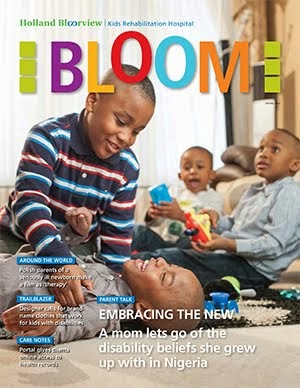
BLOOM MAGAZINE
Followers
Labels
- 1p36 deletion
- 3D printing
- A Family Like Mine
- A Family Like Mine; video; disability; Parent-talk; cerebral palsy; arts; siblings; accessibility; adulthood; services
- ABC
- ableism
- above-knee amputation
- abuse
- acceptance
- accessibility
- accessible
- accessible washrooms
- accessories
- accommodation
- Acquired disabilities
- acquired disability
- adapted sports
- adaptive living
- Adaptive-living
- ADHD
- adoption
- adult children
- adulthood
- advertising
- advertising; disability; stigma
- advertising; disability; stigma; endangered species; stereotypes; Down syndrome; disability;
- advocacy
- aggression
- airline
- Alanna Mitchell
- alberta
- albinism
- ALS
- alternative therapies
- american sign language
- amputation
- amputees
- angelman syndrome
- anger
- antidepressants
- antipsychotics
- anxiety
- app
- Applied behaviour analysis (ABA therapy)
- apraxia
- art
- Art Heals Health
- art therapy
- art; Personal stories; parenting; disability; adulthood; wheelchairs;
- arthrogryposis
- artificial intelligence
- arts
- Aspergers
- assistive devices
- attendants
- attention deficit
- attention deficit hyperactivity disorder
- audiobooks
- Augmentative and Alternative Communication (AAC)
- austerity cuts
- autism
- autism; diagnosis; pediatricians
- autism; staff stories
- autoimmune encephalitis
- avoidance
- Awards and accolades
- awareness
- Azrieli Foundation
- babies
- backpacking
- baseball
- Batten disease
- battle
- BBC Ouch
- Becoming Bulletproof
- behaviour
- behaviour therapy
- Bell Let's Talk
- bereavement
- best interests
- Beyond The Spectrum
- biking
- bioethics
- bipolar disorder
- birth defects
- black history
- black mothers
- blame
- blenderized diet
- blind
- blindness
- blog
- BLOOM
- BLOOM media round up
- BLOOM survey
- Blue Lagoon
- books
- braces
- braille
- brain
- Brain injury
- brain tumour
- brain-computer interface
- Brandie Weikle
- Brazil
- Britain
- building
- bullying
- bureaucracy
- burnout
- camp
- Canada
- cancer
- cancer; parenting; Parent-talk; hospitalization; pain; anxiety; Emotions and coping;
- cane
- capitalism
- car seat
- care farming
- care plans
- care workers
- caregivers
- caregiving
- cartoons
- Cathay Pacific
- CBC Radio The Doc Project
- Centennial College
- cerbral palsy
- cerebral palsy
- cerebral palsy; Latest-research; aging; depression; anxiety; intellectual disability; adulthood;
- cerebral palsy; parenting; disability; hearing loss; Parent-talk; negligence; jaundice; kernicterus; advocacy;
- Chatham
- Child abuse
- child death
- child ethics
- child loss
- children
- children's books
- children's books; art; graphic short stories; disability; parenting; teasing; social exclusion; inclusion; grandparents;
- Children's Hospital
- children's rehab
- China
- Choices
- christmas
- Christmas tree
- chromosome 18
- chronic fatigue
- chronic illness
- chronic pain
- chronic stress
- church
- circle of support
- cleft palate
- Clemens August Graf von Galen
- clinical care
- clinical geneticist
- Clinical-care
- clothes
- clothing
- cochlear implant
- cochlear implants
- cognitive behaviour therapy (CBT)
- cognitive development
- college
- comics
- communication
- communication and writing aids
- community
- Community Living
- compassion fatigue
- complaints
- complex medical needs
- complex medical problems
- compliments
- concussion
- Congenital Central Hypoventilation Syndrome
- Connor Sparrowhawk
- consent
- contest
- conversion disorder
- Coping and Emotions
- Cornelia de Lange syndrome
- cost of care
- costs
- costumes
- counselling
- courage
- Craig Davidson
- craniofacial condition
- Craniometaphyseal Dysplasia
- criminal justice
- critically ill children
- crowd-sourced
- Culture
- cure
- cystic fibrosis
- dads
- dance
- Dave Roche
- David Green
- day program
- deafness
- death
- death of a child
- decorations
- deep brain stimulation
- Deer Park Public School
- degenerative
- dementia
- Dene artist
- dentist
- dentistry
- depression
- design
- developing world
- development
- developmental delay
- Developmental disabilities
- developmental disability
- developmental pediatrics
- diabetes
- diagnosis
- dietitian
- direct funding
- disabilities
- disability
- disability hate
- Disability Parade NYC
- disability rights
- disability; art; books; inclusion; parenting;
- disability; arts; comics; stigma; representation; cerebral palsy;
- disability; Coping and emotions
- disability; media; language; journalism; representation;
- disability; nursing; rehab; Staff-stories; parenting
- disabled actors
- disabled parenting
- disabled parents
- discrimination
- distance learning
- diversity
- divorce
- DNA testing
- doctor-assisted suicide
- doctors
- documentaries
- Down syndrome
- Dr. Allan Peterkin
- Dr. Brian Goldman
- dreams
- drowning
- dual diagnosis
- Duchenne muscular dystrophy
- dying
- dyslexia
- dystonia
- e-letter
- early death
- early learning
- Easter Seals
- easy intervention
- echolalia
- economy
- education
- ehlers danlos syndrome
- electric shocks
- electronic health record
- emotional health
- emotions
- Emotions and coping
- empathy
- employment
- engineering
- entrepreneur
- epilepsy
- equipment
- equity
- estrogen
- ethics
- eugenics
- Europe
- euthanasia
- exclusion
- exercise
- explaining disability
- facial difference
- facilitated communication
- failure to thrive
- family
- family advisor
- family-centred care
- fashion
- fathers
- feedback
- feeding tubes
- Fiat Chrysler
- fibromyalgia
- Fiddlehead Care Farm
- film
- filmpossible
- fine-motor problems
- Firefly Books
- First in the World Somewhere
- fitness
- flight
- forced labour
- foster care
- found poetry
- Fragile X
- France
- freedom
- friendship
- funded services
- funding
- fundraising
- future
- g-tube
- Galactosemia
- gaming
- gardening
- Gaucher disease
- gender
- gender non-conforming
- genetic disorders
- genetic testing
- gifted
- global developmental delay
- grandparents
- grants
- grief
- GRIN1
- group home
- group homes
- growing up
- growth attenuation
- guide dogs
- Guillain Barré Syndrome
- guilt
- halloween
- happiness
- hate crime
- health
- health care
- health economics
- health equity
- health equity; advocacy
- health; developmental disability; autism; Down syndrome; stigma; accommodations; intellectual disability; early death; repeat emergency room visits; repeat hospital admissions; long-term care
- healthcare decision-making
- healthcare systems
- heart attack
- Hector and the Search for Happiness
- hiking
- hiring
- holidays
- Holland Bloorview
- Holocaust
- home care
- homeschooling
- hope
- hospice
- hospitalization
- housekeeping
- housing
- human rights
- human value
- human worth
- humanities
- Hungary
- hysterectomy
- identity
- illness
- imaging
- immigrant families
- immigration
- immune system
- implicit bias
- In the news
- In-the-news
- incivility
- inclusion
- incontinence
- independence
- Independent Living Fund
- Indigenous
- infection prevention
- inquest
- inspirations
- institutionalization
- Intellectual disabilities
- intellectual disability
- intelligence
- Intensive behavioural intervention (IBI)
- international
- international day of persons with disabilities
- interracial
- invisible disability
- IQ
- isolation room
- jacobsen syndrome
- Jeep
- Jerry Seinfeld
- jonathan mooney
- Journal of Pediatric Nursing
- Katherine Schneider Journalism Award
- kayaking
- Kenya
- kindness
- knitting
- L'Arche
- Langer Giedion Syndrome
- language
- Latest Research
- Latest-research
- Latest-research; Emotions and Coping; disability; parenting; autism; cerebral palsy; intellectual disability; family wellbeing
- law
- LCHAD
- learning disabilities
- legal aid
- letterboard
- LGBTQ
- library
- life planning
- life skills
- life-limiting
- lifejacket
- LIGHTS
- limb difference
- literacy
- locked facilities
- London Health Sciences Centre
- love
- Love You Forever
- low-vision
- Maayan Ziv
- magazine
- Magikme
- Magnus Cards
- maid of honour
- Maine
- make work project
- Malignant Metaphor: Confronting Cancer Myths
- marginalization
- marketing
- marriage
- massacre
- mast cell activation syndrome
- mastectomy
- McCune-Albright syndrome/fibrous dysplasia
- McMaster University
- media
- Medicaid
- medical decisions
- medical education
- medical error
- medical errors
- medical technology
- medical trauma
- medically-complex children
- medication side effects
- memoir
- Mencap
- meningitis
- mental health
- mental health; depression; anxiety; Coping and Emotions
- mental illness
- Merrywood
- metaphor
- Michael Enright
- milestones
- mindfulness
- Ministry of Community and Social Services
- missed appointments
- mobility
- moebius syndrome
- mortality
- mother blame
- mothering
- mothers
- movies
- MRI
- multiple disabilities
- multiple sclerosis
- muscular dystrophy
- Music
- music therapy
- music therapy; parenting; seizures; disability; hospitalization; trauma; Emotions and coping;
- Nadia Hamilton
- narrative medicine
- narrative training
- National Health Services
- Nature
- nature-therapy
- Nazi Germany
- near drowning
- neglect
- neonatal intensive care unit
- neonatology
- neuroblastoma
- neurodegenerative
- neurodevelopmental disorders
- neurological
- neurological impairment
- neuroscience
- NeuroTribes
- Neutropenia
- New York Magazine
- newborns
- newcomers
- NHS
- NICU
- Nike
- no-shows
- non-speaking
- non-verbal
- normal
- normalcy
- nurse practitioner
- nursery school
- nurses
- nursing
- nursing; Latest-research
- nutrition
- Nydia Langill
- obesity
- obsessive compulsive disorder
- occupational therapy
- online education
- online gaming
- ontario
- oppositional defiant disorder
- organic farming
- orthotics
- osteogenesis imperfecta
- overweight
- pain
- palliative care
- paperwork
- Para Pan Am Games
- paracanoe
- paralympics
- paralyzed
- Parapan Am Games
- paraplegia
- parent support
- Parent talk
- parent-led intervention
- Parent-talk
- Parent-talk mental health
- parenting
- parenting; disability; Snoezelen; fun; Emotions and coping;
- parenting; disability; stroke; aneurysm; rehab; family-centred care; Coping and Emotions
- pareting
- parking fees
- patient safety
- patient-centred care
- patients
- pediatric intensive care
- peer support
- Peer Support Best Practice Toolkit
- Pelizaeus-Merzbacher disease (PMD)
- Penny Pepper
- perfection
- perfectionism
- performer
- permanent residence
- person- and family-centred care
- personal floatation device
- Personal stories
- Peter Halby
- Philanthropy
- philosophy
- photography
- physical activity
- Physical disabilities
- physical education
- physiotherapy
- pictures
- pierre robin sequence
- pilot
- PKAN
- play
- play-based therapy
- playground
- playroom
- playtime
- poet
- poetry
- poetry; parenting; Parent-talk; non-speaking; language; disability; cerebral palsy; reading; coping and emotions;
- polio
- Pompe disease
- post-traumatic stress disorder
- poverty
- Prader-Willi Syndrome
- Precious Cargo
- pregnancy
- pregnancy loss
- premature babies
- prenatal health
- prenatal substance abuse
- prenatal testing
- prenatal testing; discrimination; disability; parenting; Down syndrome; advertising;
- preschoolers
- presents
- pressure sores
- preventable death
- prognosis
- promotional
- prosthetic knee
- prosthetics
- psychotherapy
- quadriplegia
- qualitative research
- quality
- quality of life
- race
- racism
- rare diseases
- rare genetic syndromes
- reading
- reception
- recreation
- Red Hot Chili Peppers
- reflux
- refugee
- registered nurses
- rehab
- relationships
- relaxation
- relaxed theatre
- Renegades
- repetitive behaviours
- reporting
- research
- residency
- residential care
- resilience
- resources
- respite
- restraint
- rett syndrome
- reverse-integration
- ride-on toy cars
- risk
- Robert Hoge
- Robert Munsch
- Role-model
- Rosemary Kennedy
- rudeness
- running
- safety
- Santa
- saving money
- school
- science
- scoliosis
- segregation
- seizures
- self-care
- self-compassion
- self-harm
- service dogs
- services
- severe disabilities
- sex
- sexism
- sexual assault
- sexuality
- shared decision making
- shoes
- shopping
- short bus
- sibling support
- Sibling-talk
- siblings
- siblings; chronic illness; emotions and coping; anxiety; panic;
- SickKids
- sight reading
- sign language
- single dads
- single moms
- single parenting
- single parents
- skeletal dysplasia
- sledge hockey
- sleep
- sleepovers
- slurs
- smiles
- social isolation
- social enterprise
- social entrepreneur
- social isolation
- social media
- social work
- social work; Staff-stories; parenting; disability; acquired brain injury; orthopedic surgery; spinal-cord injury; resilience; Coping and Emotions
- Spartan races
- special education
- special needs
- special-needs
- speech
- speech therapy
- Speechless
- spina bifida
- spinal cord injury
- spinal muscular atrophy
- Spiral Garden
- sport
- sports
- staff stories
- Staff-stories
- Staff-stories; orthopedic surgery; teaching; patient and family-centred care; cerebral palsy; emotions;
- stereotype
- stereotypes
- Steve Silberman
- stigma
- stigma; parenting
- stillborn
- stories
- storytelling
- stress
- stroke
- students
- Sturge Weber syndrome
- success
- suffering
- suicide
- Sunday Edition
- Sunshine Foundation of Canada
- support network
- surgery
- surrogate parents
- swimming
- Tanya Workman
- tapir
- teaching
- teamwork
- teasing
- technology
- TED Talks
- teens
- textile art
- The New Family
- The New York Times
- theatre
- therapeutic clown; Coping and Emotions
- therapeutic clowns
- therapy
- therapy animals
- tics
- TIFF Kids International Film Festival
- Tokyo
- Tokyo massacre
- Toronto
- Toronto Blue Jays
- Tourette syndrome
- toy shopping
- toys
- Trailblazer
- transgender; parenting
- transition
- transplants
- transportation
- trauma
- traumatic stress
- travel
- Trisomy 13
- trisomy 18
- TV
- TVO
- twins
- two blind brothers
- Ubuntu Made
- uncontrolled movements
- Undeniable
- unexpected deaths
- unhappiness; worry;
- United Nations
- university
- University of Toronto
- vegetative state
- ventilators
- Vermont
- Video
- video games
- violence
- vision loss
- Vogue
- voice device
- Voices of Youth
- volunteering
- vulnerability
- wait times
- walker
- walking
- Walt Disney
- wash-up station
- water
- We're the Superhumans
- website
- weight
- weight gain
- weight loss
- wellness
- What Happened To Your Face
- wheelchair
- wheelchairs
- Whistler Adaptive
- Who I Run For
- Williams syndrome
- Winnipeg
- withdrawal of care
- worf hirschhorn syndrome
- work-life balance
- workplace inclusion
- writing
- X Ambassadors
- X-Ambassadors
- Young Carers Program
- young filmmakers
- Zeno Mountain Farm
- Zika
- zoo
Blog Archive
-
▼
2011
(222)
-
▼
January
(18)
- What should I ask Donna Thomson?
- Word wall
- Don't forget to sign up for summer camp!
- An inspiring voice
- Ethics in the NICU
- Jan. 26 update
- What is a life well lived?
- My name is Matt
- Growing up
- Individual Education Plans 101
- Game to boost fitness, friendship
- No advance, no retreat
- Homeschooling: How I did it
- The gift of grace
- Welcome to Zach's List
- 'Good things can happen'
- An education
- Learning to love the baby steps
-
▼
January
(18)
-
Disclaimer
Content in BLOOM is not a substitute for professional medical advice. Always consult your doctor.
Views expressed in posts and resources listed do not signify endorsement by Holland Bloorview Kids Rehabilitation Hospital.
The BLOOM blog welcomes comments from readers on issues that affect parents of children with disabilities. We moderate comments to ensure they’re on-topic and respectful. We don’t post comments that attack people or organizations.
Holland Bloorview Kids Rehabilitation Hospital
150 Kilgour Road, Toronto Ontario Canada M4G 1R8 Get directions
Tel 416 425 6220 - Toll free 800 363 2440 - Fax 416 425 6591
Copyright © Holland Bloorview Kids Rehabilitation Hospital. 2014. All Rights Reserved.























1 comments:
Thank you for posting Louise. I believe that the medical history of Trisomy 13 and 18 is very important for the future of all children with genetic conditions.
When these conditions were first identified back in the 60's, large population studies revealed that the rate of survival was greater than it is now. Think about that. The 60's were the dark ages of neonatology. How could the stats have gotten worse? Would this have occurred if there was no associated disability?
Once the condition was identified and the child was labeled, there was certainty of disability and it appears that treatments were withheld. These children clearly did not benefit from the major advances in neonatology available to other children. Stories abound related to terminal sedation and infants pushed off into the corner of nurseries and left without food to "mercifully die" as soon as possible. Eventually, these early deaths, of which many could have been prevented, contributed to dismal survival statistics and these conditions were erroneously labeled as "lethal" and "incompatible with life." Like a self-fulfilling prophecy, many children died because they were expected to die and were thus denied standard care.
There is no doubt that many of these children are best treated with comfort care. But there is a vast range that exists. All children and families are unique.
In my opinion, the situation with trisomy 13 and 18 represents a potential dark side of prenatal genetics, including inappropriate labeling. Once a prenatal test exists if the majority choose termination, do options and choices for children born cease to exist? As a society, with public health care based in part on "majority values" is this acceptable?
Dr. Mercurio made an excellent statement about questioning the validity of standards and protocols:
"Good medical practice requires knowing the strength of the evidence and arguments that support any standard, and basing one's degree of flexibility with regard to the standard on the strength of its foundation. A similar point could be made with regard to ethical questions in medicine: our obligation to adhere to a standard of care should be greatly informed by the strength of the data and the ethical reasoning that support that standard."
There is much that is not known about trisomy 13 and 18. Thanks to the internet, the parents are becoming empowered. They are determined to ensure that the truth of the value and beauty of their children's lives, however long, be known and that their children should be medically treated as individuals, not as genetic labels.
Post a Comment